Hong Kong has recorded zero deaths in care homes from Covid-19 by employing strict infection control measures that were ignored in the UK, MPs were told on Tuesday as the death toll from the virus in English and Welsh care homes reached almost 15,000.
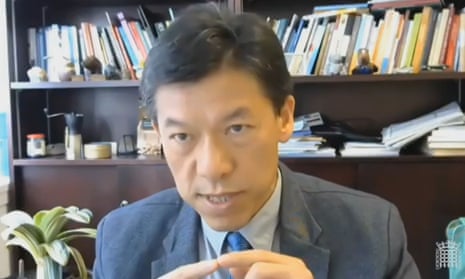
Despite sharing a border with China, Prof Terry Lum, the head of social care policy at Hong Kong University, told the UK parliament’s health and social care select committee that Hong Kong treated the outbreak like Sars, the killer virus that hit Asia in 2003, and saved lives.
By contrast, the UK’s response to coronavirus was based on planning for a flu pandemic.
TimelineThe coronavirus crisis in care homes in England and Wales
Show
Public Health England issues guidance stating that it was “very unlikely” care homes would become infected. The guidance was not withdrawn until 12 March.
Despite a lack of official statistics about fatalities, care homes warn that they are at “breaking point” and MHA, the country’s biggest charitable provider, says it has suspected cases in more than half of its facilities.
The Department of Health and Social are guidelines on discharging hospital patients into care homes states: “Negative tests are not required prior to transfers/admissions into the care home.”
Chief medical adviser Chris Whitty says that more than one in ten care homes (13.5%) now has at least one case of Covid-19. Whitty says: “Care homes are one of the areas where there are large numbers of vulnerable people and that is an area of risk and therefore we would very much like to have much more extensive testing.”
Testing is expanded into care homes but only for people with symptoms.
Five of the largest care home providers say they have now recorded a total of at least 1,052 deaths
Care home deaths are included alongside deaths in hospitals after a sharp rise of more than 4,300 deaths over a fortnight in England and Wales. Testing is extended to staff and residents without symptoms.
Launch of a national delivery system for personal protective equipment to care homes is hit by a delay of up to three weeks
Academics report that more than 22,000 care home residents in England and Wales may have died as a direct or indirect result of Covid-19 – more than double the number stated in official figures.
An unpublished government study which used genome tracking to investigate outbreaks revealed that temporary care workers transmitted Covid-19 between care homes as cases surged. In evidence raising further questions about ministers’ claims to have “thrown a protective ring around care homes”, it emerged that agency workers – often employed on zero-hours contracts – unwittingly spread the infection as the pandemic grew, according to the study by Public Health England.
A report by care homes bosses says that thousands of people lost their lives “prematurely” because care homes in England lacked the protective equipment and financial resources to cope with the coronavirus outbreak.
Care leaders, unions and MPs round on prime minister Boris Johnson after he accuses care homes of failing to follow proper procedures amid the coronavirus crisis, saying the prime minister appeared to be shifting the blame for the high death toll.
Lum said care facilities in Hong Kong had been highly vigilant against spread from hospitals with any confirmed cases quarantined for up to three months.
This contrasted with evidence from Prof Martin Green, the chief executive of Care England, which represents the largest provider networks, who said asymptomatic and symptomatic Covid-19 patients were discharged from hospitals into care homes spreading the virus.
“Most important is stopping the transmission from hospital to nursing home,” Lum said. “We do a very good job on isolation. Once we have any person infected we isolate them in hospital for three months and at the same time we isolate all the close contact people in a separate quarantine centre for 14 days for observation.
“They do tests regularly in that 14 days to make sure they don’t have the virus. We use a supercomputer to trace the close contacts of people being infected particularly for cluster outbreaks.”
He added that all nursing homes had a trained infection controller and underwent emergency drills simulating an infection outbreak four times a year so infection control becomes “a well-worn practice”.
Lum’s account came as the health and social care committee tried to learn lessons from the crisis in care homes, where four in 10 Covid deaths have occurred. Its chairman, Jeremy Hunt, described estimates that 22,000 people may have died from Covid and related issues in care homes as “very, very shocking”.
MPs also heard from Isabell Halletz, the chief executive at the German employers’ association for care homes, who said there had been fewer than 3,000 Covid-19 deaths in care homes in Germany, partly because no one was allowed in from hospitals without a negative test, or had undergone quarantine in designated centres or repurposed hotels for at least 14 days.
Adelina Comas-Herrera, a research fellow at the London School of Economics studying Covid-19 deaths in care homes globally, also praised Singapore and South Korea, which have recorded no care home deaths by quarantining infected residents or moving them to hospitals.
“[Their] infection control policies [were] based not on influenza but on Sars and that has helped them,” she said.
The international comparisons came as figures released by the Office of National Statistics on Tuesday revealed 9,980 deaths were registered in care homes in England and Wales up to 8 May from confirmed or suspected Covid-19. Adding more up-to-date death tolls reported to regulators and deaths of care home residents in hospitals to 1 May, it means 14,835 care residents have died from Covid-19.
UK care homes are demanding a significant increase in testing of staff and residents, up to three times a week, amid fears a lifting of the lockdown could spark new outbreaks.
So far, the UK health secretary, Matt Hancock, has promised only that all care home residents and staff will be tested by 6 June, but no commitment has been made for repeat testing.
“People are often finding their tests aren’t arriving on time or being taken away on time,” said Green. “We are looking at delays of eight to 10 days until people get results.”
The call for routine testing was echoed by Sir David Behan, the chief executive of HC-One, the largest private provider, and Sam Monaghan, the chief executive of MHA, the largest charitable provider.
Vic Rayner, the executive director at the National Care Forum, which represents charitable care operators, said the promise of 30,000 tests a day was enough only for one test each for care residents and staff.
“What that means is you haven’t got the right tools and resources to manage outbreaks within homes and identify when and where infections might have come in,” she said. “It’s incredibly challenging for providers to operate in that climate. It is absolutely critical that we get that repeat testing.”
The committee also heard warnings about the continued risk posed by temporary care workers spreading the virus if they work in more than one home. A Public Health England study, revealed by the Guardian on Monday, found this had happened in early April but instructions to restrict movements were issued by the government only last Thursday.
Green said floating agency staff were a danger and operators may have to ensure agency staff are restricted to a particular care home rather than move between care homes.
James Bullion, the president of the Association of Directors of Social Services, said: “The fact that we have agency staff moving between three or four establishments is a consequence of the structural model we have got. We do need to look at a salaried model and higher level of wages.”