What the development of penicillin tells us about developing a coronavirus vaccine
By Dan Drollette Jr | May 18, 2020
In 2004, Eric Lax wrote a well-regarded book about the development of penicillin, the world’s first so-called miracle drug. Titled “The Mold in Dr. Florey’s Coat,” it made a complicated scientific topic accessible to a lay audience—and helped set the record straight about penicillin’s development. It also illuminated how much labor, time, money, technology, inspiration, and sheer luck went into the creation of penicillin. And it delved into the complicated interplay of personalities involved, or what The Guardian called “good fortune and squabbling” in its review of the book. In this interview, the Bulletin’s Dan Drollette Jr finds out what parallels—and differences—exist between the pressure to develop penicillin during World War II and the demand by public figures today for a vaccine to take out the coronavirus. And if we may be banking too much on a magic bullet to end the coronavirus pandemic in a few months.
(Editor’s note: This interview has been condensed and edited for length and clarity.)
Drollette: I was wondering what we all could learn about developing a coronavirus vaccine from the penicillin experience—if there are any parallels so far as science, government, philanthropy, and private enterprise go. But I realize the comparison isn’t be perfect—penicillin is an antibiotic, not a vaccine. Can you explain, in layperson’s terms, the difference between an antibiotic and a coronavirus vaccine?
Lax: With any antibiotic, such as penicillin, you’re talking about something being used to fight off organisms like bacteria—complex, single-celled creatures with cell walls, that can reproduce on their own. The antibiotic attacks the bacteria, and the disease the bacteria causes, that’s in you right at this moment. And you generally use penicillin, or any antibiotic, just once for a particular case—at most, you get a shot or two, or maybe a shot and a booster.
This means that every time you get a streptococcal bacteria infection, for example, you’ve got to take the penicillin again.
But a virus is a whole different kind of thing to go after. It’s much tinier than a bacteria, cannot survive long on its own, and can only reproduce by attaching itself to a host. It is really more of a chunk of genetic material—a blueprint—that reprograms the cells of its host to make new viruses.
And while antibiotics can kill bacteria, they don’t work against viruses.
Consequently, we treat a virus differently, typically through the use of a vaccine. You essentially try to train your body’s immune system to develop the ability to recognize and attack a particular viral invader, so your body knows to bring out its defenses and get rid of the virus on its own—to develop what we call immunity.
Once your body is able to identify the virus as a threat, it will always recognize something pretty close to that virus when it comes back. So you’re set for life… for that one particular virus.
The problem being that there are many different viruses—and there’s always a new virus coming out, so it’s an arms race between the viruses and your immune system.
So what a vaccine is doing is really a matter of getting the body to recognize the virus for what it is: an invader, a pathogen, the bad guy. And your body does the fighting against it.
While an antibiotic like penicillin fights the thing directly itself.
But there are similarities—and dissimilarities—in how we go about developing something that fights against bacteria, and something that helps us fight viruses.
Drollette: How did you wind up doing a book about penicillin’s development?
Lax: I was reading The New York Times one morning and saw a lengthy obituary of a New Haven woman named Anne Miller. The Times had given her death two entire columns and a picture, because she was the first American to be treated with penicillin, and restored by it.
The more I read the obit, the stranger it became. Because I, like so many people, had always associated penicillin—the first so-called miracle drug—with Alexander Fleming.
But the more I read Miller’s obituary, the more I realized that Fleming didn’t really make it into the useful drug we know. Instead, that came about because of this small group of people at Oxford University, headed by someone named Howard Florey, about a dozen years later. But the obit didn’t go into much more—just enough to whet my appetite about penicillin’s origins. And there was that phrase: “First American saved by penicillin.”
But what really made this the book happen was that one of the main folks on the Oxford University research team, Norman Heatley, was still alive—though in his late ‘80s.
And I was able to get an interview with him for an hour, which became lunch, and then dinner. I wound up spending the next three days with him. In fact, for the next year, while I was deep into book research—I spent about a week per month in London—I always went down to see him; his stories were so good. But he’s the guy who figured out the whole process that allows us to get production of this drug in large volumes—which actually solved the penicillin problem.
About two-thirds of the way through, I discovered that Heatley was a great diarist. His diaries tell about everything going on in the lab, and about a secret wartime trip to America on the Pan Am Clipper—the Concorde of its time. The diary gave the full range of experience; for example, it describes how he fell in love with somebody in America and then had to leave her. It had all of these elements that make it real and human, as opposed to “We did this experiment.”
Drollette: It must have been something to pick his brains. Which gets to my next question: How long did it take to do this book?
Lax: A couple of years for research alone. But I’ve never had more fun researching a book.
Luckily, a large majority of the letters, lab notes, and other relevant papers were in one place, at the Royal Society in London, on the Mall opposite from Buckingham Palace.
So, I would go to the Royal Society every morning at 10 o’clock when they opened. And they’d bring up these boxes of papers they had about the development of penicillin, and every one was like opening a package at Christmas. I mean, each one had an abstract of what was supposed to be inside, but you never really knew what to expect when you opened it.
And later each morning, you would hear “clip, clop, clip, clop” and realize that was the sound of the Horse Guards riding by, on their way to the Changing of the Guard.
Drollette: The book gave the impression that there were many twists, turns, and blind alleys in developing penicillin; there was no obvious series of sequential steps, where A led to B which led to C. Is that a fair summary?
Lax: I think so, yes. And you have to consider the technology they had in the 1930s and 1940s. Any first-rate middle school today has a better-equipped lab than they did. So they basically often had to make what they needed from scratch.
But I think that Heatley is the guy who stood out in this regard, for his ability to come up with novel solutions.
For example, he had a notion of how they could scale up from their original process of extracting penicillin from mold—which involved doing a lot of things by hand with dozens of dishes of various sizes and shapes. So he came up with a sort of Rube Goldberg device, with bottles, glass tubes, and old clock parts, which he gathered from the town dump.
To modern eyes, the end result really was high-school science fair type stuff—glass tubing in the stairwells, running all the way from the roof to the ground level.

Drollette: Any similarities between finding penicillin then and finding a coronavirus vaccine today?
Lax: Researchers still have to make big conceptual leaps. And we need that kind of thinking once again; this is such a peculiar virus in so many ways, with all the strange side effects it’s having: children showing signs of heart attacks, or otherwise healthy 39-year-olds getting blood clots.
So, the fundamental nature of science is still the same; you’re still problem-solving.
Drollette: How long did it take, from the time that people first thought about using penicillin as an antibiotic to it actually being given to patients?
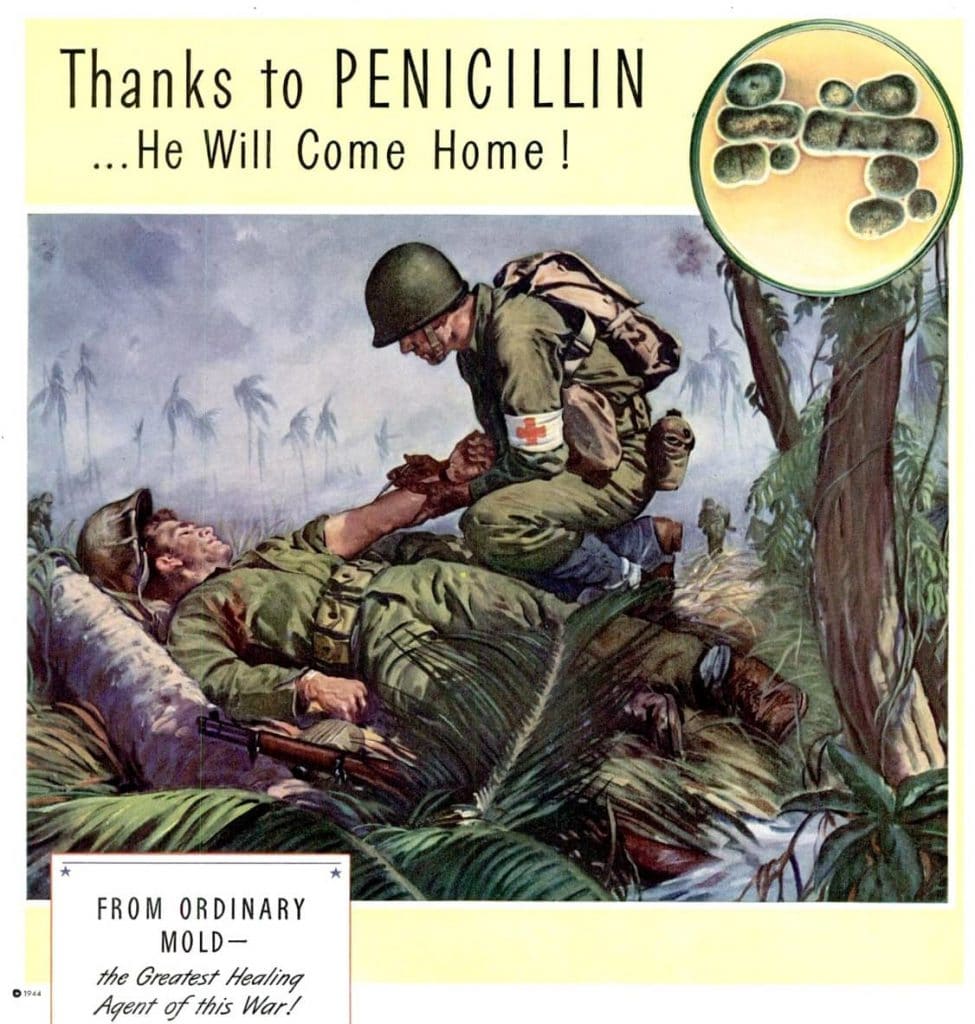
Lax: Over 20 years, and even that was sort of by accident. I mean, in the 1920s Alexander Fleming noticed a certain strain of mold seemed to kill organisms, but he didn’t know what to do with it; he thought penicillin might be a great tool for cleaning glassware.
It took a team of scientists at Oxford—Howard Florey, Norman Heatley, and Ernst Chain—to read about this laboratory curiosity, realize the potential it had to kill the organisms that cause bacterial infections, and do the research to make it into a great antibiotic.
Which was sorely needed, because in those days people used to die from minor infections caused by something as simple as getting a blister or a splinter. Literally, a scratch from a rose thorn could start a staphylococcus infection that would lead to death. Before antibiotics arrived, we were subject to any number of diseases that could just lay you out in a second: diphtheria, typhus, typhoid, tuberculosis.
And then it turned out that Penicillium notatum—this extract from mold—had within it the wonderful capability to attack deadly bacteria.
But even after discovering its potential, this team of British scientists still had to get it to grow in quantities large enough to be studied, identify the active ingredient, purify it, test it—safely—on people to make sure it had no unwanted side effects, then figure out how to make it on an industrial scale and distribute it. All under wartime conditions, with Hitler poised to invade England at any moment.
And a key item was producing large enough quantities to be useful.
Drollette: Quantity is that important?
Lax: Oh, yes. The war was such a needy time for an antibiotic, and lots of it; people still remembered the impact of sepsis in World War I. And for centuries before that, the diseases and infections associated with war were more deadly than the actual fighting. (In the American Civil War, twice as many soldiers died of disease as from battle). There was a point, in 1942 or ‘43, when the number two item on the US War Department’s wishlist was mass production of an antibiotic like penicillin. Number one was the atomic bomb.
And remember, there was no guarantee they’d be successful in getting penicillin to work; antibiotics had proved so elusive before. The most promising ones—sulfa drugs—had turned out to be such a disappointment.
Drollette: So it took 20-odd years for penicillin to go from laboratory curiosity to something that could be used to cure patients?
Lax: It’s hard to pinpoint, because penicillin languished in obscurity for a good 10 years, before Ernst Chain read about it and brought it up before his colleagues. They then started working on it in the lab in 1939, so it was maybe five or six years from then to something widely used.
Drollette: If penicillin took that long, do you think it’s a bit rushed to expect we’ll have a coronavirus vaccine in a few months?
Lax: At a minimum, I’d say it’s the height of optimism, or even magical thinking. It’s more a matter of years than a few months.
Although I have heard that some folks at the Jenner Institute [Oxford University’s nonprofit vaccine research unit] may have clinical trials of a coronavirus vaccine relatively soon, based on work they’d already been doing on a similar coronavirus from last year. They’re starting preliminary trials now. So something may be available by sometime in 2021, which would just be extraordinary.
But I think a key point to remember is that the reason why Jenner’s having some luck is because they’ve been working on coronaviruses over the last 10 or 12 years. And so they can build off it.

Drollette: But even that timescale is not as short as what the Trump administration is pitching, for a coronavirus vaccine before November or December?
Lax: Yes. This is not my field of expertise, but if you based this on history, that’s never happened before—to get something up and working to counter a disease within the same year of the outbreak. It’s one thing to get the DNA code on the disease, but then you’ve got to test your cure, and test it, and test it. And then ramp up production and make sure that you’re meeting a standard where one dose really is the same as the other dose, and all on a massive scale.
Drollette: So getting large volumes of the drug or vaccine is not cut-and-dried?
Lax: Not if we’re going by the history of penicillin. What the English folks at Oxford came up with for penicillin in the 1940s was a basically two-dimensional process: You have a couple inches of liquid and grow a mold on top of it, which you then harvest and purify. It was terribly slow.
And then they showed their work to American pharmaceutical companies, who came up with the great idea of getting the mold to grow all throughout the depth of the entire column of liquid in a vat, rather than just at the very surface—what are called brewing techniques, and still used today. It was like strapping an aqualung onto the back of all of the penicillin spores in the liquid, because they were suddenly getting fed everywhere. Each penicillin spore could get bigger and reproduce much more easily because it was getting the oxygen it needed. So far as ramping up goes, that discovery was really major.
The other thing that shouldn’t be overlooked in how this happened so fast and so well—and so fortuitously for the war—is the simple, wonderful good luck of the relationship between the head of the Oxford team, Howard Florey, and a key person on the American side, physiologist John Fulton from Yale.
Fulton had been a Rhodes scholar with Florey at Oxford and they had hit it off very well; later, Fulton and his wife would look after the Florey children during the war, when kids were evacuated so as to be out of harm’s way during the Battle of Britain.
Fulton was incredibly well-connected to everybody in science and well-regarded. So when Heatley and Florey wanted to fly over to the States with their small sample of penicillin, the Ford Foundation arranged for them to go on the fastest transportation available at the time. By chance, they arrive on a July 4 weekend, and Fulton is able to invite a who’s who of scientists to his place for a July 4th party.
So Heatley and Florey can go around and spread the word about this thing called penicillin at this party. And then, a few days later, Fulton arranges for them to go down to Washington and see everybody—meaning that every door in science and government is open.
Plus, they have the Ford Foundation on their side.
Just think of it: These guys get off the plane in New York. The next day, they’re up in New Haven, where Fulton’s put together this huge thing. The next week, they’re doing Washington. Within 10 days, they’ve seen everybody, and there’s a plan for what to do. They’re seeing all of the drug companies. They’ve got people in the highest positions in government behind them.
Suddenly, this is fast-tracked.
If it had been two people from Cambridge coming over without these connections, the creation of penicillin probably would’ve been much more difficult and much slower. Who knows how long it would have taken?
So because of these personal relationships, from the moment they hit the ground, they’re off and running. And they’ve got Vannevar Bush—head of all wartime military research and development, including the early phases of the Manhattan Project—on their side. I mean, Florey and Heatley really have the entire US government establishment behind them.
There really was a coordinated effort, between the federal government, science, industry, and nonprofits like the Rockefeller and the Ford foundations. They were all headed in the same direction, pulling together.
Drollette: It seems so different from today. There was an article in the New York Times just a few days ago; the title tells you everything: “Trump’s Response to Virus Reflects Long Disregard for Science.”
Lax: I simply don’t understand the decisions he’s made; he seems so cavalier about the value of science. I mean, why cut back on science at a time that we need it more than ever? There was all of the prep work that we had at the ready for this, so why do you close that office? Where is the federal response for testing and masks and materials and helping to get vital supplies? Why is this the states’ problems?
This event is why you have a federal government, for organizing responses to a crisis like this. Nothing makes any sense to me.
You can’t rely on private enterprise alone to tackle this, it takes about $2 billion for a pharmaceutical company to bring something to market.
Drollette: And yet I’ve seen headlines like “DOW surges more than 400 points as positive Gilead news lifts hope for coronavirus treatment” and “Administration describes a dash for a coronavirus vaccine.” It seems they’re overemphasizing how quickly things can happen.

Lax: I’d love to see them break the record and have a vaccine out in a year. I hope they have it tomorrow.
But there were so many happy accidents involved in bringing penicillin to market: getting the federal government to back the effort to research and develop it, and then getting the pharmaceutical companies on board, to name just a few.
I just hope that all the good fortune and serendipity that happened around penicillin can happen again, because we need it to look for a vaccine against coronavirus. We need every good thing, every bit of cooperation, every entity pulling together, every person seeing the importance of this. Our lives really depend on this.
Together, we make the world safer.
The Bulletin elevates expert voices above the noise. But as an independent nonprofit organization, our operations depend on the support of readers like you. Help us continue to deliver quality journalism that holds leaders accountable. Your support of our work at any level is important. In return, we promise our coverage will be understandable, influential, vigilant, solution-oriented, and fair-minded. Together we can make a difference.
Keywords: COVID-19, Coronavirus, penicillin, pharmaceuticals, vaccines
Topics: Analysis, Biosecurity, Special Topics